Balance billing prohibited for health care facility services
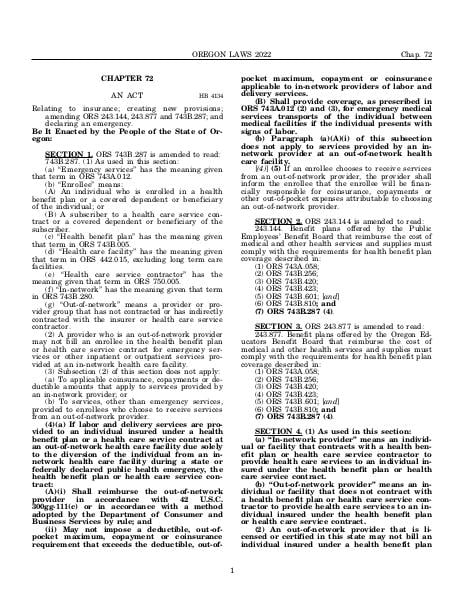
Amended by HB 4134
Effective since March 23, 2022
Relating to insurance; creating new provisions; amending ORS 243.144, 243.877 and 743B.287; and declaring an emergency.
Source:
Section 743B.287 — Balance billing prohibited for health care facility services, https://www.oregonlegislature.gov/bills_laws/ors/ors743B.html.